Prevalence Of Cannabis Use Disorder In The United States
Cannabis is the most widely used psychoactive substance in the United States . Based on the 2018 National Survey on Drug Use and Health, an estimated 43.5 million people, ages 12 and older, used cannabis in the last year in the United States, which equates to an estimated 15.9% of the population. During 2018, the prevalence of cannabis use in the past year was highest among those 18 to 25 years of age . The use of marijuana has steadily increased since 2002, and there has been a trend towards legalization in several states .
Statistics On Marijuana Addiction And Abuse
is a psychoactive drug which comes from a THC-bearing plant. It is becoming increasingly legal throughout the US, both for medicine and for recreation, but its still not completely safe because it may be addictive and cause health problems.
- About 30-40 million Americans smoke Marijuana every year.
- About 43% of American adults admit to trying Marijuana.
- About 30% of people who regularly use Marijuana have a Marijuana use disorder.
- The average batch of Marijuana in 1990 contained less than 4% THC, but that percentage has since risen to over 12%.
- Roughly 10% of all Marijuana users will become addicted to the drug.
- Around 17% of all who start using the drug as minors become addicted.
Stimulant Use Among Individuals With Opioid Use Disorder
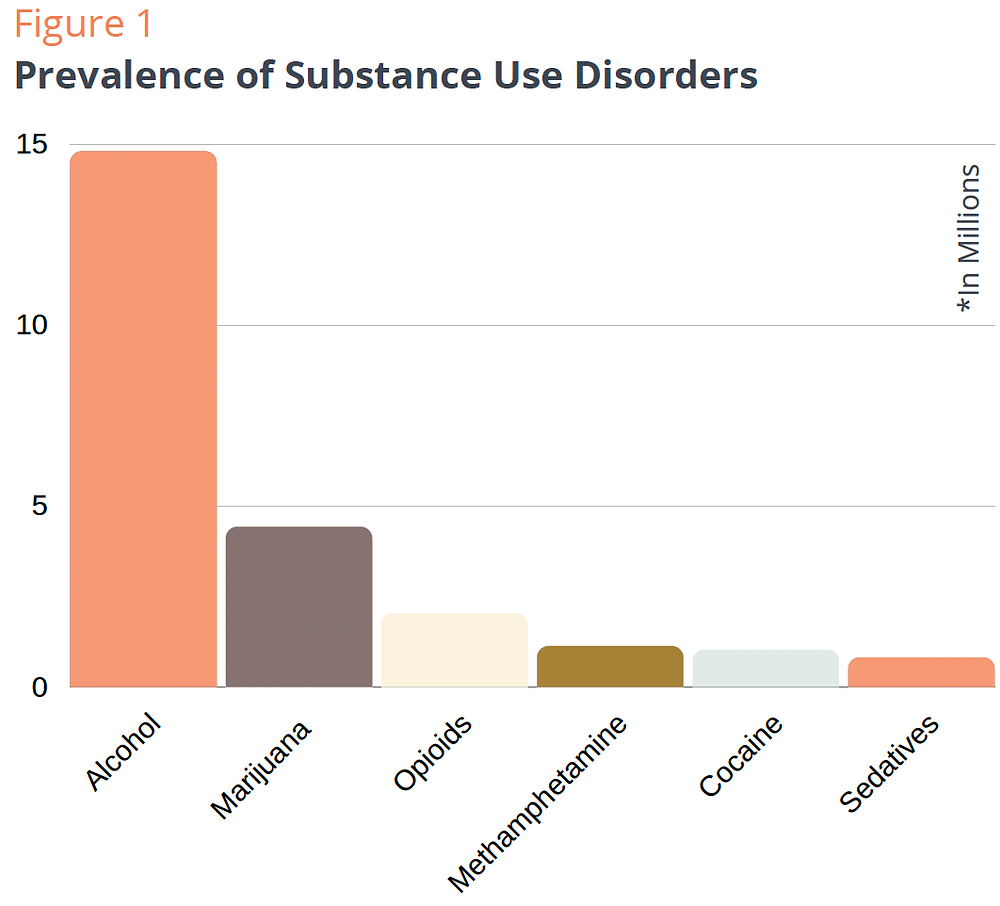
As shown in Figure 1, lifetime exposure to stimulants was very high among this sample of individuals with opioid use disorder, with 82.4% reporting the use of prescription stimulants, crack/cocaine or methamphetamine, after adjusting for time since initial drug exposure to an opioid or stimulant. Crack/cocaine had the highest adjusted rate of lifetime use , followed by methamphetamines and prescription stimulants .
Figure 1. Prevalence of lifetime exposure to opioid and stimulants among individuals with opioid use disorder , adjusted for age of initial drug exposure and time since year of initial drug exposure.
Respondents were categorized by the year of initial drug exposure to either an opioid or a stimulant and grouped into 5 year blocs across the past 30 years, from 1991 to 2020. Figure 2 depicts lifetime use of opioid and stimulant categories by respondent’s year of initial drug exposure. Of those who initiated use from 1991 to 2010, lifetime use of all three stimulant categories were reported by over half the sample 54.058.5% for prescription stimulants, 68.368.2% for methamphetamines, and 80.366.0% for crack/cocaine. These rates were lower in more recent years with just 5.1% exposed to prescription stimulants, and 1213% to crack/cocaine and methamphetamines, by 20162020.
Figure 2. Prevalence of lifetime exposure to opioids and stimulants grouped by year of initial drug exposure among individuals with opioid use disorder.
Don’t Miss: Can Drug Addiction Cause Narcissism
Statistics On Cocaine Addiction And Abuse
Cocaine is an illegal Stimulant. Whether it comes in the form of powder or crystal , Cocaine can damage organs, provoke mental disorders, and cause respiratory failure. Cocaine is also highly addictive. Some Cocaine users may become addicted after using the drug only once.
- About 5 million Americans are regular Cocaine users.
- A little under 2% of 8th graders had used Cocaine as of 2020.
- In 2020, almost 1% of 8th graders had used Crack.
- Cocaine-related fatalities have grown every year since 2013.
- There were 14,666 such deaths in 2018.
- Americans between the ages of 18 to 25 use Cocaine more than any other age group.
The Trouble With Time And Terminology

To understand how this confusion came about, we need to go back in time. Since 1952, the American Psychiatric Association has published several editions of its Diagnostic and Statistical Manual of Mental Disorders , a classification of psychiatric diagnoses. Over the years, as the understanding of various psychological disorders has changed, the association has updated this widely accepted manual. In the early editions, the APA referred to addictive disorders as addictions. But in 1994, the fourth edition replaced the term addiction with dependence, apparently with a goal of using a less pejorative word.² Thus, an addict was considered to be dependent on a drug, so that a heroin addict was termed opioid dependent. Ever since, dependence has remained the preferred term for professionals when describing addiction.
Both the DSM-4 criteria, as well as the current DSM-5 version released in 2013, require three elements to diagnose substance use disorder :
-
loss of control
-
continuation despite significant adverse consequences
-
preoccupation or obsession with obtaining, using, and recovering from the effect of the substance.
But the term dependence, meaning addiction, was so entrenched by then that even the FDA in 2016, as shown in the language used in their approval of ,¹ was still using the term dependence when they meant addiction. In fact, they approved Probuphine for the treatment of Opioid Use Disorder which is how the drug is used in practice today.
You May Like: How Strong Is Nicotine Addiction
Strategy To Address Stigma
There is not yet strong evidence pointing to strategies that effectively reduce stigma against people with OUD among health care professionals. However, emerging literature does illustrate some promising directions, and action to address this barrier is imperative. Targeted education early in training can abate stigmatizing attitudes, such as pessimism or uncertainty on the effectiveness of treatment, perceptions that caring for people with SUD is not rewarding, perceptions that patients who abuse substances are difficult and unpleasant, and beliefs that OUD treatment resides outside the domain of medical practice . Highlighting the efficacy of medications, portraying SUD as treatable conditions, and illustrating sympathetic personal narratives of people who use drugs are also strategies that can reduce stigmatization by the general population against people who use drugs .Finally, academic detailing is an interactive educational strategy that involves visits to health care providers by trained professionals who can provide tailored training and technical assistance. It has been used to train physicians to engage in evidence-based opioid prescribing and to support pharmacists starting to distribute naloxone to the public . It is possible that the use of academic detailing may reduce stigma while equipping providers to offer MOUD.
Demographic Psychosocial And Clinical Variables
Survey demographic items included gender , age, race, employment, education, marital status, and living arrangement. Psychosocial items were asked in reference to the past 12 months. Homelessness was defined as living on the street, in a shelter, in a single room occupancy hotel, or in a car. Food insecurity was assessed using an item from the Health Leads Social Determinants of Health Screening Tool . Recent discrimination in healthcare settings for substance use was assessed by the following question: In the past 12 months, have you ever felt you were treated unfairly getting health care services because of your drug and/or alcohol use? For psychiatric comorbidity , one item asked: Have you ever had or been treated for depression, anxiety, post-traumatic stress disorder, or any other psychiatric condition? Healthcare access was defined as seeing a provider other than an addiction provider at least once in past 12 months. The Medical Outcomes Study Social Support Survey measured social support using a 6-point frequency scale higher average scores indicate more social support . Number of previous substance use treatment episodes was also assessed.
Recommended Reading: How Long Does It Take To Get Addicted To Xanax
A Brief History Of Opioid Addiction Terminology
Based on the Diagnostic and Statistical Manual of Mental Disorders , of the American Psychiatric Association
-
1952 1993: The DSM I, II, and III, termed addictive substance disorders, including opioid addiction, as addiction.
-
1994: The DSM-4 relabeled substance addiction as dependence meaning a heroin addict would be called opioid dependent.
-
2013: The DSM-5 introduced the term Opioid Use Disorder to describe opioid addiction. Addiction overall was replaced by Substance Use Disorder. The term dependence was dropped from the manual altogether neither opioid dependence nor drug dependence can be found in its extensive index. Given that the main characteristic of physical dependence is the presentation of withdrawal symptoms upon stopping the substance, the DSM-5 does note that withdrawal is one of the 11 criteria for diagnosing OUD, stating: This criterion is not considered to be met for those individuals taking opioids solely under appropriate medical supervision. In other words, the APA is noting that physical dependence is not a criterion for addiction in patients being prescribed opioids.
For more on this topic, see PPM’s 2019 .
Related
Signs Of An Opioid Overdose
Every year, thousands of deaths in the United States are attributed to opioid overdose. If you fear that someone has overdosed on opioids, call 9-1-1 right away. Signs that someone may have overdosed include:
- Loss of consciousness
- Slow and erratic pulse or no pulse
- Irregular breathing or no breathing
- Face is very pale and/or clammy
- Pupils are constricted
- Body is limp
Read Also: What Are People Addicted To
Enhancing Healthcare Team Outcomes
While opioid use disorder is on the rise across the world and has transformed into an epidemic in the U.S., it needs a better understanding from healthcare professionals and government intervention along with resources and a team-based approach to managing these patients. It requires an interprofessional approach where the cognitive and behavior therapies need to be supported by medical intervention to reduce the chances of withdrawal and relapse. Medications are available to use in pregnancy and have shown better neonatal outcomes, as well as improve morbidity and mortality in the adult population.
The primary care physician is responsible for coordinating the care, which includes the following:
Furthermore, the possibility of addiction, dependence and withdrawal symptoms must merit consideration when treating opioid use disorder. An interprofessional team working together can reduce the morbidity and mortality of chronic opioid use and overdose. Naloxone can be a life-saving treatment for a patient on chronic opioids. The long-term outcomes for detoxification and drug rehabilitation are promising.
Treatment Considerations For Persons With Hiv
There are limited clinical trial data on pharmacotherapy for smoking cessation among persons with HIV. Available data suggest that varenicline is safe and effective in persons with HIV. The Adult and Adolescent ARV Guidelines support recommendations for smoking cessation as provided by the USPSTF and suggest that clinicians should consider evidence-based behavioral and pharmacotherapy strategies to promote smoking cessation and maximize survival among persons with HIV. In general, pharmacotherapies used for smoking cessation have few drug interactions with HIV medications and can be used safely with most first-line antiretroviral regimens the one major exception is that coadministration of bupropion with medications that are CYP2B6 inducers, such as efavirenz, lopinavir, and ritonavir, can reduce levels of bupropion.
Read Also: What Is The Disease Model Of Addiction
Alcohol Use Disorder Medications
Acamprosate, disulfiram, and naltrexone are the most common medications used to treat alcohol use disorder. They do not provide a cure for the disorder, but are most effective in people who participate in a MAT program. Learn more about the impact of alcohol misuse.
Learn more about MAT for alcohol use disorders and view Medication for the Treatment of Alcohol Use Disorder: A Brief Guide 2015.
How To Communicate About Addiction And Dependence With Patients And Caregivers
Understanding the neurobiology of addiction and dependence can be invaluable knowledge to the prescribing healthcare professional. By understanding what influences patient behaviors, clinicians can better determine rational goals and expectations.¹¹ Accordingly, providing patients with this information helps to reduce the stigma associated with addiction and dependence.
For individuals with chronic pain who require opioids, open communication between clinician and patient is key in ensuring safety and reduce barriers to care. Prior to initiation of chronic opioid therapy, having an honest discussion about both the potential benefits and risks of opioids, including physical dependence, tolerance, addiction, withdrawal, and OUD can help individuals make informed decisions about their health and treatment.
Discuss dependence, tolerance, and withdrawal as side effects of opioid use which are due to chemical changes in the body. Additionally, help the patient understand the physical, psychological, and behavioral mechanism of OUD as a mental health disorder so that they feel comfortable discussing cravings and related thoughts or their actions with you should they begin to slip into a risky situation. As part of open communication, create a plan for discontinuation if the opioid therapy risks change to outweigh benefit that both the patient and provider agree upon.
Read Also: What To Say To An Addict
What Causes Opioid Use Disorder
Genetic and environmental factors play a role in the development of opioid use disorder. These drugs are also easy to access.
Additionally, some prescription opioids tend to take effect quickly and are extremely potent. This makes them more addictive. People who mix other mind-altering substances, including alcohol, have a higher risk of developing an addiction.
In some cases, opioid addiction begins with a doctors prescription of the drug.
Medications For Opioid Addiction Include:
- Available as dissolving tablet, cheek film, extended-release injection, or 6-month implant under the skin.
- Can be prescribed by a doctor for use outside of a clinic.
- Can only be used in a certified opioid treatment program setting.
- Can be prescribed by any clinician who can legally prescribe medication.
- Only used for people who have not used opioids for at least 710 days.
Talk with a doctor to find out what types of treatments are available in your area and what options are best for you and/or your loved one. Addiction is a chronic, relapsing disease be sure to ask your doctor about the risk of relapse and overdose.
If you notice that someone may be struggling with opioid addiction:
Also Check: How Long Does It Take To Get Over An Addiction
Opioid Misuse By Income And Education
Across the U.S., nearly 50 percent of adults with OUD have low incomes and nearly 25 percent live in poverty. Some studies have also found a link between rising OUD rates and bad economic times, such as the Great Recession at the end of the 2000s. This is thought to be one reason for the increase in opioid misuse in the Northeast in the years that followed.
Opioid use varies by education and employment, but can still affect anyone:
- 4.2 percent of people with some college or an associateâs degree misuse opioids. Thatâs a higher rate than that of both college graduates and those who didnât finish high school.
- 7 percent of unemployed adults, 3.9 percent of full-time employees, and 3.6 percent of part-time employees misuse opioids.
Improving Access To Evidence
ABSTRACT |Even though evidence-based treatment for opioid use disorders is effective, almost four in five Americans with OUD do not receive any form of treatment. The gap in access to evidence-based care, including treatment with medications for OUD, stems in part from barriers to change within the health care system. This paper includes nine key barriers that prevent access to evidence-based care, including stigma inadequate clinical training a dearth of addiction specialists lack of integration of MOUD provision in practice regulatory, statutory, and data sharing restrictions and financial barriers. Action from a number of actors is urgently needed to address this crisis.
Don’t Miss: Where To Get Free Help For Drug Addiction
Some Of The Painkiller Substance
Opioid The term opioid refers to natural and synthetic substances, which mainly acts on three of the receptor systems . The way of consuming it involves:
- Intranasal use snorting or sniffing
- Intravenous use shooting up or mainlining
- Subcutaneous use skin-popping
- Intramuscular use muscling
Heroin Heroin is the opioid most commonly abused by injection. Its chemical name is diacetylmorphine, which is a derivative of morphine, another commonly used opioid. Other terms for heroin include dope, horse, smack, china white, junk, and tar.
Opium It is obtained from the opium poppy, which contains morphine and codeine. It is consumed through smoking, and it can be eaten, too. The usage of opium is very low in the United States and it is the most commonly abused substance in Asia and the Middle East.
Endorphin It is often referred to as a subclass of opioids, which contains endogenous peptides that relieve pain.
Prescribed Opioids Medications containing opioids were prescribed principally for pain relief. But they have the potential for abuse and addiction, hence the usage of prescription drugs is monitored and regulated by the Controlled Substances Act in the United States.
Opiates It is also referred to as a subclass of opioids, which contains alkaloid compounds that are naturally present in opium poppy.
Synthetic Opioids Synthetic opioids are fentanyl, tramadol, and methadone, whereas the semi-synthetic opioids are Oxycodone and hydrocodone.
David A Fiellin Md Internal Medicine
The idea of treating opioid addiction without medication is attractive, especially because such programs can be effective for some patients with alcohol use disorder. A lot of people think that the goal of treatment for opioid use disorder is not taking any medication at all. However, the truth is that the many people in abstinence only programs for opioid use disorder will relapse. Research shows that medication-based treatments are the most effective treatment. Opioid use disorder is a medical condition just like depression, diabetes or hypertension, and just like those conditions, it is most effectively treated with a combination of medication and counseling.
There are two common medications used to treat opioid use disorder: methadone and buprenorphine. These medications help address patients withdrawal symptoms and block the reward or the high that people get from using opioids. They help restore normal brain functioning. In certain cases, other medications can help improve impulse control and treat any underlying psychiatric disorders.
Recommended Reading: How To Fight Alcohol Addiction
Defining Opioid Dependence And Addiction
Confusion surrounding the definitions of addiction and dependence is not new. The complicated history of opioid addiction terminology is discussed in a previous practical pain management . The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition describes, what previous editions of the DSM have described dependence as a symptom of SUD, along with impaired control, social problems, and risky use.
Dependence, noted in DSM-5, is a symptom of SUD, and is labeled as a side effect of chronic opioid use when used appropriately for chronic pain however, dependence alone does not singularly indicate an SUD diagnosis. Opioid dependence is a physical reaction to chronic opioid use where withdrawal is precipitated upon abrupt discontinuation.
People with SUD and OUD experience changes in brain chemistry and structure in areas that relate to judgement, decision-making, learning, memory, and behavioral control.¹ Education of the mechanisms for SUD and dependence in addition to communicating these mechanism with patients and their family members is key in mitigating stigma and improving patient care.
