What Is Substance Use And Addiction
Many people use substances such as drugs or alcohol to relax, have fun, experiment, or cope with stressors, however, for some people the use of substances or engaging in certain behaviours can become problematic and may lead to dependence.
Addiction is a complex process where problematic patterns of substance use or behaviours can interfere with a persons life. Addiction can be broadly defined as a condition that leads to a compulsive engagement with a stimuli, despite negative consequences.i This can lead to physical and/or psychological dependence. Addictions can be either substance related or process-related, also known as behavioural addictions .ii Both can disrupt an individuals ability to maintain a healthy life, but there are numerous support and treatment options available.
A simple way of understanding and describing addiction is to use the 4Cs approach:
- Loss of control of amount or frequency of use
- Compulsion to use
- Continued substance use despite consequencesiii
How common is substance use and addiction?
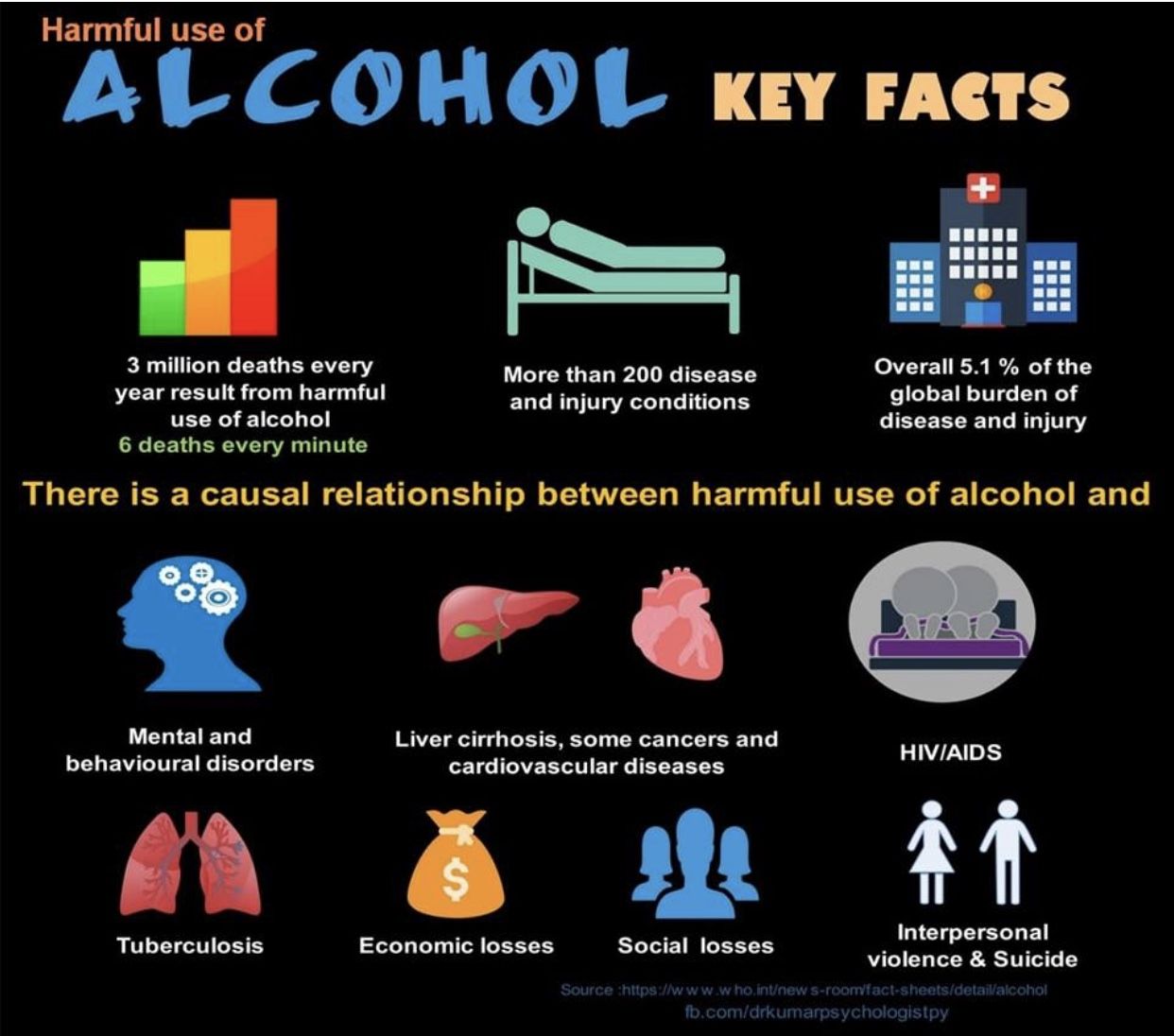
Substance use is quite common on an international scale and statistics vary depending on the substance being consumed. It is estimated that nearly 5% of the worlds population have used an illicit substance, 240 million people around the world use alcohol problematically, and approximately 15 million people use injection drugs.iv
Perceptions Of Mental Health
Canadians with a mental or substance use disorder within the past year were less likely to rate their mental health as positive during the same time frame, compared with those who did not have a mental or substance use disorder . Approximately 29.6% of those with a mental or substance use disorder perceived their mental health as very good or excellent. This finding may partly reflect the episodic nature of these disorders, since they can occur between periods of good health.
People with a profile consistent with substance use disorder rated their mental health much higher than those with mood disorder or generalized anxiety disorder. A higher proportion of people with substance use disorder rated their mental health as excellent or very good , compared to those with mood disorder or generalized anxiety disorder whose self-evaluations of mental health were roughly the same.
The Link Between Substance Abuse And Mental Health
When you have both a substance abuse problem and a mental health issue such as depression, bipolar disorder, or anxiety, it is called a co-occurring disorder or dual diagnosis. Dealing with substance abuse, alcoholism, or drug addiction is never easy, and its even more difficult when youre also struggling with mental health problems.
In co-occurring disorders, both the mental health issue and the drug or alcohol addiction have their own unique symptoms that may get in the way of your ability to function at work or school, maintain a stable home life, handle lifes difficulties, and relate to others. To make the situation more complicated, the co-occurring disorders also affect each other. When a mental health problem goes untreated, the substance abuse problem usually gets worse. And when alcohol or drug abuse increases, mental health problems usually increase too.
Co-occurring substance abuse problems and mental health issues are more common than many people realize. According to reports published in the Journal of the American Medical Association:
- Roughly 50 percent of individuals with severe mental disorders are affected by substance abuse.
- 37 percent of alcohol abusers and 53 percent of drug abusers also have at least one serious mental illness.
- Of all people diagnosed as mentally ill, 29 percent abuse alcohol or drugs.
Affordable Online Therapy
Need urgent help? .
Also Check: How To Know Your Addicted To Something
Initiation Of Cocaine Use
Among people aged 12 or older, the number of past year initiates of cocaine use decreased from 1.0 million in 2002 to 671,000 in 2019 .39 This number in 2019 was lower than the numbers in 2002 to 2007 and in 2015 to 2018, but it was similar to the numbers in 2008 to 2014. The number of people aged 12 or older in 2019 who initiated cocaine use averaged to about 1,800 people each day . Continued monitoring of trends for initiation of cocaine use is important for assessing progress in preventing people from trying cocaine.
Figure 29. Past Year Cocaine Initiates among People Aged 12 or Older: 2002-2019
+ Difference between this estimate and the 2019 estimate is statistically significant at the .05 level.
| Age |
|---|
| 135 |
| + Difference between this estimate and the 2019 estimate is statistically significant at the .05 level. |
Among adolescents aged 12 to 17, the number of past year initiates of cocaine use decreased from 310,000 in 2002 to 59,000 in 2019 . This number in 2019 was lower than the numbers in most years from 2002 through 2017, but it was similar to the number in 2018. The number of adolescents in 2019 who initiated cocaine use averaged to about 160 adolescents each day .
Perceived Need For Substance Use Treatment
NSDUH respondents were classified as having a perceived need for substance use treatment if they indicated that they felt they needed substance use treatment in the past year. Respondents may have a perceived need for substance use treatment, regardless of whether they had an SUD in the past year. In this report, estimates for the perceived need for substance use treatment are discussed only for people aged 12 or older who were classified as having an SUD in the past year70 but did not receive substance use treatment at a specialty facility.68,69
Among the 18.9 million people aged 12 or older in 2019 with an SUD in the past year who did not receive treatment at a specialty facility, 95.7 percent did not feel that they needed treatment, 3.0 percent felt that they needed treatment but did not make an effort to get treatment, and 1.2 percent felt that they needed treatment and made an effort to get treatment .71 Among people aged 12 or older in 2019 with a past year SUD who did not receive substance use treatment at a specialty facility, 4.3 percent perceived that they needed treatment.71 This percentage in 2019 was similar to the percentages in most years from 2015 to 2018.
Figure 70. Perceived Need for Substance Use Treatment among People Aged 12 or Older with a Past Year Substance Use Disorder Who Did Not Receive Substance Use Treatment at a Specialty Facility in the Past Year: 2019
Aged 12 to 17
Aged 18 to 25
Aged 26 or Older
Don’t Miss: Pain Meds For Recovering Addicts
Integrated Treatment And Care Of People With Dual Diagnoses
Effective management of either substance use disorders or mental health disorders is challenging. Dual diagnosis adds complexity to assessment, diagnosis, treatment and recovery, and can be associated with increased incidences of relapse, poorer physical health, and risks of homelessness, violence and other challenges.
Research suggests that people with a dual diagnosis respond well to integrated programs that address both their mental illness and their substance misuse. Treatment can help people manage their alcohol or drug use, improve physical and mental health, and improve their general functioning.
However, these programs were uncommon until recent years. Some of the reasons for this include:
Importantly, people who experience dual diagnosis are affected in different ways and therefore have individual needs. In practice, what is effective for one person may not be effective for another.
Mde And Mde With Severe Impairment Among Adults
Among adults aged 18 or older, the percentage with a past year MDE increased from 6.6 percent in 2005 to 7.8 percent in 2019 . These estimates in 2019 were higher than the estimates in each year from 2005 through 2018.
Figure 49. Major Depressive Episode in the Past Year among Adults Aged 18 or Older: 2005-2019
+ Difference between this estimate and the 2019 estimate is statistically significant at the .05 level.
| Age |
|---|
| 4.7 |
| + Difference between this estimate and the 2019 estimate is statistically significant at the .05 level. |
Among adults aged 18 or older, the percentage who had a past year MDE with severe impairment increased from 4.0 percent in 2009 to 5.3 percent in 2019 . These estimates in 2019 were higher than the estimates in each year from 2009 through 2018.
Figure 50. Major Depressive Episode with Severe Impairment in the Past Year among Adults Aged 18 or Older: 2009-2019
+ Difference between this estimate and the 2019 estimate is statistically significant at the .05 level.
| Age |
|---|
| 3.2 |
| + Difference between this estimate and the 2019 estimate is statistically significant at the .05 level. |
Aged 18 to 25
Aged 26 to 49
Aged 50 or Older
Don’t Miss: How To Cure An Addictive Personality
Cdc Mental Health Statistics
Observations In the CDC findings, with very few exceptions, there is a clear trend between the beginning and end of the survey period with everything trending upwards for the 18-29, 30-39,40-50 age brackets. For participants in the 50-59, 60-69, 70-79, and 80+ age groups, there was either very little change, or in some cases an improvement.
NEGATIVE TRENDS
| 8.5 | 25 |
Here we see that while the actuals differ for both males and females the two biggest increases are
- Received therapy / counselling
- Needed but didnt get therapy / counselling
For the group which didnt get the therapy or counselling they believe they should have, the increase for males was 35.9% more than it was for the female respondents.
Kratom Use In The Past Month
Kratom is an herbal extract from the leaves of the Mitragyna speciosa tree that is native to Southeast Asia. The leaves contain chemicals with mind-altering effects. Kratom can come in forms such as powders, pills, or leaves.23,24 The 2019 NSDUH asked respondents aged 12 or older about their use of kratom in the 30 days before the interview. Among people aged 12 or older in 2019, 0.3 percent used kratom in the past month . In addition, 0.1 percent of adolescents aged 12 to 17 , 0.5 percent of young adults aged 18 to 25 , and 0.3 percent of adults aged 26 or older used kratom in the past month .
Recommended Reading: How To Help People With Drug Addiction
Any Mental Health Service Use Among Adults With Ami
Among adults aged 18 or older with past year AMI, receipt of mental health services in the past year increased from 40.9 percent in 2008 to 44.8 percent in 2019 . This percentage in 2019 was higher than the percentages in 2008 to 2012, but it was similar to the percentages in most years from 2013 through 2018.
Figure 75. Any Mental Health Services Received in the Past Year among Adults Aged 18 or Older with Any Mental Illness in the Past Year: 2008-2019
+ Difference between this estimate and the 2019 estimate is statistically significant at the .05 level.
| Age |
|---|
| + Difference between this estimate and the 2019 estimate is statistically significant at the .05 level. |
Aged 18 to 25
Among young adults aged 18 to 25 with past year AMI, receipt of mental health services in the past year increased from 30.3 percent in 2008 to 38.9 percent in 2019 . This percentage in 2019 was higher than the percentages in 2008 to 2016, but it was similar to the percentages in 2017 and 2018.
Aged 26 to 49
Among adults aged 26 to 49 with past year AMI, receipt of mental health services in the past year increased from 41.4 percent in 2008 to 45.4 percent in 2019 . This percentage in 2019 was higher than the percentages in most years from 2008 to 2012, but it was similar to the percentages in 2013 to 2018.
Aged 50 or Older
Drug Abuse Treatment & Prevention
Beginning in the early 2010s, states that began to enhance their prescription drug monitoring programs saw drastic results.
- Between 2010 and 2015, Kentucky saw an 85% decrease in the number of opioids prescribed per person.
- In 2010, Florida stopped health care providers from dispensing prescription opioid pain medication from their office locations alongside a PDMP and in 2012, marked a 50% decline in oxycodone overdose deaths.
- In 2012, New York required prescribers of medication to check the states PDMP before prescribing opioids and in 2013, marked a 75% drop in patients who went to multiple doctors/prescribers for the same drugs.
- There has been a 16% annual decline in nationwide opioid prescriptions.
- The rate of Americans receiving medication-assisted treatment increases 13% annually.
- In 2018, nearly 19 million people aged 12 and older needed substance abuse treatment.
- 964,000 perceived a need for treatment, 392,000 went on to seek treatment.
- 946,000 adolescents aged 12-17 needed substance abuse treatment, 159,00 received treatment.
- 5.2 million young adults or 1 in 7 aged 18-25 needed substance abuse treatment, only 1.6% or 547,000 received treatment.
- 15.1 million adults or 1 in 14 aged 26 or older needed substance abuse treatment, only 1.4% or 3 million received treatment.
Recommended Reading: How Do People Get Addicted To Heroin
Rates By Age Groups And Sex 12
In 2012, rates of mood disorders and substance use disorders for the 12 months prior to the survey tended to be lower in older age groups. Mood disorders, for both males and females, were highest among youth aged 15 to 24 , and lowest for those aged 65 and older . Substance use disorders followed a similar pattern highest among youth and lowest among adults aged 45 and over . Youth have been commonly found in other studies have higher 12-month rates of mood disorders and substance use disorders than older age groups.Note 9 Similarly, low rates of disorders among those aged 65 and older is a common pattern found in other research. Note 10, 11
In 2012, females had a higher rate of depression within the previous 12 months , than males . Females also had higher rates of depression than males in all age groups except among those aged 65 and older, where the rates were similar .
For both males and females, rates of depression within the past year were highest among youth aged 15 to 24, and lowest among those aged 65 and older. The largest difference between males and females was in the youngest age group, where among those aged 15 to 24, 9.0% of females met the criteria for depression, compared with 5.3% of males.
Caffeine Intoxication And Withdrawal
Caffeine intoxication and caffeine withdrawal are included in DSM-5. Caffeine use disorder, however, is in the section of DSM-5 for conditions requiring further research. While there is evidence to support this as a disorder, experts conclude it is not yet clear to what extent it is a clinically significant disorder.
Don’t Miss: How Can Addiction Be Prevented
Principles Of Effective Drug Addiction Treatment
These 13 principles of effective drug addiction treatment were developed based on three decades of scientific research. Research shows that treatment can help drug-addicted individuals stop drug use, avoid relapse and successfully recover their lives.
Initiation Of Inhalant Use
Among people aged 12 or older in 2019, 730,000 people initiated inhalant use in the past year , which was higher than the numbers in 2016 to 2018 but was similar to the number in 2015 . The number of people aged 12 or older in 2019 who initiated inhalant use in the past year averaged to about 2,000 people each day .
Among adolescents aged 12 to 17 in 2019, 381,000 people initiated inhalant use in the past year, which was higher than the numbers in 2016 and 2017, but it was similar to the numbers in 2015 and 2018 . The number of adolescents in 2019 who initiated inhalant use in the past year averaged to about 1,000 adolescents each day .
Among young adults aged 18 to 25, the number of past year initiates of inhalant use remained stable between 2015 and 2019 . In 2019, 250,000 young adults initiated inhalant use in the past year, or an average of about 690 new inhalant users aged 18 to 25 each day .
Among adults aged 26 or older, the number of past year initiates of inhalant use remained stable between 2015 and 2019 . Among this population in 2019, 99,000 people initiated inhalant use in the past year, or an average of about 270 new inhalant users aged 26 or older each day .
You May Like: How To Know If You Are Addicted To Weed
